Testicular sperm extraction (TESE) and microdissection TESE (microTESE) are advanced procedures in reproductive medicine designed to retrieve sperm directly from the testes in men with severe male factor infertility. These techniques are particularly valuable for men with non-obstructive azoospermia (NOA), where sperm production is impaired and no sperm is present in the ejaculate.
TESE: Testicular Sperm Extraction
TESE is a procedure in which a small sample of testicular tissue is surgically removed to extract sperm. Here’s a closer look at its key aspects:
- Procedure: TESE involves making an incision in the scrotum to access the testicle. A small piece of testicular tissue is excised and then processed in the laboratory to extract viable sperm cells.
- Indications: TESE is primarily indicated for men with NOA, especially those who have failed to retrieve sperm through less invasive methods like percutaneous epididymal sperm aspiration (PESA) or testicular sperm aspiration (TESA).
- Expectations: The success rate of TESE varies. In general, the chances of finding sperm range from 30% to 90%, depending on the underlying condition. Sperm retrieval success rates are higher in men with obstruction, such as those after a vasectomy or having congenital bilateral absence of the vas deferens (CBAVD) or men with focal areas of sperm production, compared to those with uniform testicular failure.
microTESE: Microdissection Testicular Sperm Extraction
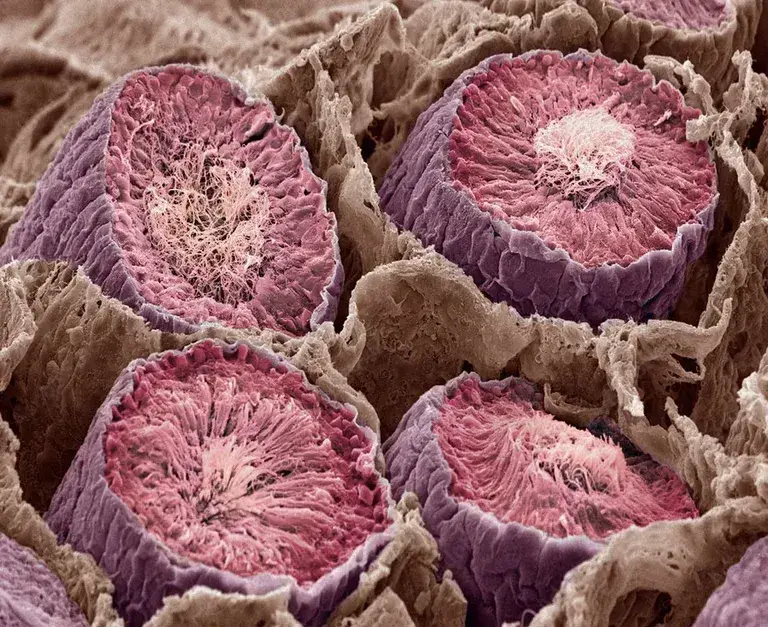
microTESE is a more refined and advanced technique that uses an operating microscope to locate areas of sperm production within the testicle. This method offers several advantages over conventional TESE:
- Procedure: microTESE is performed under an operating microscope, which allows the surgeon to identify and selectively remove the most promising areas of testicular tissue. The microscopic magnification helps in distinguishing between healthy and damaged tissue, thereby increasing the likelihood of finding viable sperm.
- Indications: microTESE is especially indicated for men with severe NOA, where sperm production is extremely limited. It is often recommended when initial attempts using TESE or other methods have failed.
- Expectations: The success rate of microTESE is generally higher than that of TESE, with sperm retrieval rates reported to be between 40% and 63%. The precision of microTESE helps in maximizing the chances of finding sperm while minimizing damage to the testicular tissue.
Banking of Tissue and Sperm: A Crucial Step
Regardless of the method used, banking the retrieved sperm and testicular tissue is essential for future fertility treatments. Here’s why:
- Future Use: Cryopreservation of sperm allows for multiple attempts at in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) without the need for repeated surgical procedures.
- Maximizing Chances: Given the variability in sperm retrieval success, banking any viable sperm found provides a valuable resource for future fertility treatments.
- Cost-Effective: Banking reduces the need for additional surgical procedures, which can be costly and invasive.
The sperm bank you choose must document the quality of the sperm present in the sample and provide you and your fertility doctors with a report and images of the sperm present. This information, particularly the images of the sperm present, provides crucial information for the technical staff preparing the testicular specimens for use in IVF (in vitro fertilization). These images provide insight into the challenges present and the time and staff that will be required for preparing the specimens for use in an IVF procedure, and in this way, significantly increase the probability of a successful outcome.
Realistic Expectations
While TESE and microTESE offer hope for men with severe male infertility, it is important to set realistic expectations:
- Variable Success Rates: Success rates can vary significantly based on individual conditions, including the underlying cause of NOA, testicular health, and prior treatments.
- Multiple Procedures: Sometimes, multiple procedures may be necessary to retrieve sufficient sperm for IVF/ICSI.
- Collaboration with Specialists: Working with experienced reproductive urologists and fertility specialists is crucial for optimizing outcomes.
Conclusion
TESE and microTESE represent significant advancements in the field of male infertility, offering hope to men who previously had limited options. While these procedures come with their challenges and variable success rates, the ability to bank sperm and tissue provides a pathway to potential parenthood. For couples facing severe male infertility, understanding these options and setting realistic expectations can be an empowering step towards achieving their dreams of having a family.
New York Cryo performs Testis Tissue processing, cryopreservation, and storage services for your surgeon for a flat fee. The services provided are listed below. Many are only available from New York Cryo.
Our Comprehensive service include:
- Intraoperative Urgent-Pak Kit – This kit is sent to your Surgeon a week before your procedure. It includes all the items needed to help ensure a successful tissue retrieval, Including sperm washing media, conical specimen tubes, patient labels, sterile tissue dissecting dishes, prelabeled slides, coverslips, and slide holders, cryovials (microTESE only), sterile specimen containers, specimen bags and an insulated IATA compliant box for transport from the operating room to New York Cryo.
- Consultation – A consultation with the patient and New York Cryo’s Medical Director to discuss the process of sperm banking, results of the semen analysis, and required infectious disease blood testing to answer frequently asked questions regarding the comparative specimen quality, specimen stability over time, and the process of releasing specimens when results.
- Physical Examination (PE) – can be performed by the referring physician or by the Medical Director of New York Cryo.
- Men’s Health Questionnaire (MHQ) – Documents the patient’s medical history
- FDA infectious disease screening Questionnaire (blood testing not included)
- Informed consenting process – reviewing and answering questions about the Stored Specimen Agreement and Consent.
- Specimen Processing – Includes basic semen analysis, processing of the specimen with freeze media, and cryopreservation
- Post-Thaw Analysis – a required test performed greater than 48 hours after the initial specimen freeze to determine sperm survival after the freeze-thaw process.
- Limited semen analysis – Performed on the initial specimen and includes:
- Volume – a measure of the amount of seminal fluid
- Concentration – the number of sperm in a specified volume of ejaculate
- Count – the total number of sperm in the specimen
- Qualitative Motility – how the sperm moves. The test includes both the percent of motile sperm as well as a measure of how fast and in what direction, they move.
- Viability testing – to assess the functional ability of sperm cells within the semen sample by determining the percentage of live and motile sperm present.
- Images/Videos of the reproductive tissue stored – essential for documentation of what is stored and invaluable for the inseminating laboratory to identify the sperm quality. Having these images often saves the patient thousands of dollars in wasted time and procedures.
- The first year of storage for up to ten vials. (multi-year discounts are available).
-
Note: Blood testing must be performed within three days of the laboratory receiving the specimen. We use LabCorp, which has FDA-approved test kits with reflex NAT testing. New York Cryo does not perform blood testing, and the costs for blood testing are not included in our Fee for sperm banking. It is the Client Depositor’s responsibility. Please check with your third-party payer to see if you will incur any out-of-pocket costs for blood testing. We can arrange for courier service. Any fees incurred will be the patient’s responsibility. Please contact us with any questions.