ADVANCEMENTS IN SPERM FREEZING: WHAT’S NEW IN MALE FERTILITY PRESERVATION
Sperm freezing, also known as sperm cryopreservation or sperm banking, has been a cornerstone of male fertility preservation for decades. Initially developed in the 1950s, the technology has evolved significantly, making sperm banking more effective, reliable, and accessible than ever. With advancements in cryopreservation techniques and improvements in assisted reproductive technologies (ART), men now have even better chances of preserving their fertility long-term.
In this blog, we’ll explore the latest advancements in sperm freezing, focusing on innovations that are improving success rates, the future of fertility preservation technologies, and how these developments benefit patients and healthcare providers.
The Basics of Sperm Freezing
Sperm freezing involves the collection, processing, and storage of sperm in liquid nitrogen at extremely low temperatures (-196°C). At this temperature, all biological activity, including cellular degradation, stops, allowing sperm to be preserved indefinitely. The frozen sperm can then be thawed and used in assisted reproductive procedures such as intrauterine insemination (IUI), in vitro fertilization (IVF), or intracytoplasmic sperm injection (ICSI).
Traditionally, sperm freezing has been an effective means of preserving fertility, especially for men undergoing medical treatments like chemotherapy or radiation, which can damage sperm production. Sperm can remain viable for decades, with successful pregnancies reported from sperm stored for over 20 years. However, continuous improvements in freezing techniques and post-thaw applications are pushing the boundaries of what is possible with cryopreservation.
Advancements in Cryopreservation Techniques
- Vitrification: A Breakthrough in Rapid Freezing
One of the most significant advancements in sperm freezing is the development of vitrification, a method that allows for the ultra-rapid freezing of sperm. Unlike traditional slow-freezing methods, which involve gradually cooling sperm to cryogenic temperatures, vitrification freezes sperm almost instantly, preventing the formation of ice crystals that can damage sperm cells.
- Why It Matters: Ice crystal formation during freezing can damage the sperm’s cellular structures, reducing their viability after thawing. Vitrification minimizes this risk by turning the sperm into a glass-like state without ice crystal formation. This technique is particularly useful for men with low sperm counts or poor-quality sperm, as it maximizes the survival of viable sperm after thawing .
- Improved Cryoprotectants
Cryoprotectants are substances added to sperm samples before freezing to protect the cells from damage during the freezing and thawing processes. Over the years, new and improved cryoprotectants have been developed that are more effective at safeguarding sperm from freezing damage.
- Why It Matters: Better cryoprotectants mean higher survival rates for sperm after thawing. These advancements allow for more viable sperm to be available for use in fertility treatments, which is especially important for men with limited sperm production or poor sperm quality.
- Microfluidic Sperm Sorting Before Freezing

Another exciting advancement in sperm preservation is the use of microfluidic sperm sorting before freezing. This technology uses tiny channels and fluid dynamics to isolate the healthiest, most motile sperm from a semen sample before it is frozen.
- Why It Matters: Microfluidic sorting allows for the selection of the best sperm, which increases the chances of successful fertilization and healthy embryo development after thawing. This method can be especially beneficial for men with low sperm quality or high levels of DNA fragmentation in their sperm. Sorting the sperm before freezing improves overall outcomes in assisted reproductive technologies (ART).
- Sperm Banking for Genetic Screening
Recent advancements in genetic screening technologies have added a new dimension to sperm freezing. Men can now opt to have their sperm genetically screened before freezing to detect potential genetic abnormalities or mutations. This screening can be especially valuable for men with known genetic disorders or those who wish to reduce the risk of passing on hereditary conditions.
- Why It Matters: By identifying genetic risks before sperm freezing, men can make informed decisions about future family planning. This advancement adds an extra layer of security for men who want to ensure that their stored sperm is of the highest quality, both in terms of viability and genetic health.
Enhanced Post-Thaw Applications for Frozen Sperm
Once frozen sperm is thawed, it can be used in a variety of assisted reproductive technologies (ART) to help achieve pregnancy. Recent advancements in ART are improving the success rates of using frozen sperm, even for men with fertility challenges.
- Intracytoplasmic Sperm Injection (ICSI)
ICSI is a technique in which a single sperm is injected directly into an egg, bypassing many of the obstacles that sperm typically face during fertilization. This method has revolutionized the use of frozen sperm, especially for men with low sperm counts or poor sperm motility.
- Why It Matters: ICSI increases the chances of successful fertilization, even when only a few viable sperm are available. This technique is particularly useful for men who have undergone sperm freezing due to cancer treatments or other medical conditions that severely impact sperm quality.
- Artificial Intelligence (AI) in Sperm Selection
Artificial intelligence (AI) is beginning to play a role in sperm selection during fertility treatments. AI algorithms can now be used to analyze sperm samples and identify the healthiest sperm for use in ICSI or IVF procedures.
- Why It Matters: AI can help select sperm with better motility, morphology, and DNA integrity, improving the chances of successful fertilization and embryo development. This technology is especially beneficial when using frozen sperm, as it helps maximize the potential of the stored sample .
- Stem Cells Derived Sperm for Future Fertility
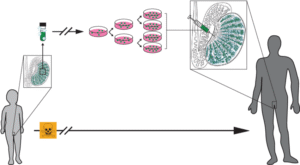
Although still in the experimental stages, research into sperm derived from stem cells holds promise for the future of male fertility preservation. Scientists are exploring the possibility of using stem cells to regenerate new sperm in men who have become infertile because of medical treatments or aging.
- Why It Matters: This groundbreaking research could one day allow men to restore their fertility, even if their sperm production has been severely compromised. While this technology is not yet available, it represents an exciting frontier in male fertility preservation.
The Future of Sperm Freezing: What’s Next?
As the field of cryopreservation continues to advance, several exciting developments are on the horizon that could further revolutionize sperm freezing and male fertility preservation.
- Nanotechnology in Cryopreservation
Nanotechnology is being explored as a way to improve the cryopreservation process by enhancing the delivery of cryoprotectants and improving the freezing and thawing procedures. By using nanoparticles, scientists hope to achieve more precise control over the freezing process, minimizing cellular damage and improving sperm survival rates.
- Automation of Sperm Freezing and Thawing
Automation is another area where sperm freezing could see significant advancements. Automated systems for sperm collection, freezing, and thawing could reduce the risk of human error and ensure more consistent results. This could also help make sperm banking more accessible and cost-effective by streamlining the process.
- Gene Editing and Fertility Preservation

As gene-editing technologies like CRISPR continue to evolve, there is potential for using these techniques to correct genetic abnormalities in sperm before freezing. This could help men with genetic disorders preserve healthy sperm for future use, reducing the risk of passing on hereditary conditions.
Who Benefits from These Advancements?
The advancements in sperm freezing and fertility preservation have far-reaching implications for various groups of men:
- Cancer Patients: Men undergoing chemotherapy or radiation can benefit from these advancements, ensuring that their fertility is preserved despite treatments that could damage sperm production.
- Men with Genetic Conditions: Men with genetic disorders or family histories of hereditary diseases can take advantage of genetic screening and potential future gene-editing technologies to preserve healthy sperm.
- Men Delaying Fatherhood: Men who wish to delay fatherhood can now bank their sperm with greater confidence, knowing that the latest cryopreservation techniques will ensure their sperm remains viable for years to come.
- Men with Low Sperm Quality: Advancements in sperm sorting, vitrification, and ICSI offer new hope for men with low sperm counts or poor sperm motility, increasing their chances of successful conception.
Conclusion
The field of sperm freezing has come a long way since its inception, with recent advancements significantly improving the process and success rates of fertility preservation. Innovations such as vitrification, microfluidic sperm sorting, and AI-driven sperm selection are pushing the boundaries of what’s possible, offering men more reliable options for preserving their fertility.
For both patients and healthcare providers, staying informed about these advancements is crucial for making the best decisions about fertility preservation. Whether due to medical treatments, age, or genetic concerns, the future of sperm freezing looks brighter than ever, providing men with the tools they need to safeguard their reproductive potential.