EVALUATION OF THE SUBFERTILE MALE: PART 3 – SEMEN ANALYSIS
Semen analysis is a cornerstone of evaluating male fertility and understanding potential causes of subfertility. It assesses multiple factors affecting sperm health, providing valuable information for healthcare providers and patients alike. This is the third of several blogs on evaluating the subfertile male. In this blog, I will cover the components of a comprehensive semen analysis, how each is measured, and why a licensed andrology laboratory is essential for accurate results. The insights gained from this analysis are pivotal in diagnosing male fertility issues and forming effective treatment plans.
Why Semen Analysis Matters
Semen analysis is one of the most informative tools for understanding male factor subfertility. It allows doctors to assess the number, movement, and shape of sperm, each of which plays a crucial role in fertility. When combined with blood testing (such as hormone levels) and imaging studies (like scrotal ultrasound), semen analysis provides a clearer picture of a man’s reproductive health. This comprehensive view helps healthcare providers recommend specific treatments that address the underlying issues most effectively.
Components of a Comprehensive Semen Analysis
A semen analysis typically measures several key components, each of which offers insights into sperm health and fertility potential. A high-quality semen analysis involves both manual and computer-aided sperm analysis (CASA) methods, ideally conducted in a licensed andrology laboratory with trained technologists.
- Volume
- What It Measures: Semen volume is the total amount of fluid in a semen sample, typically measured in milliliters (mL).
- Why It Matters: Low semen volume (hypospermia) may indicate issues with the seminal vesicles or prostate gland, which contribute fluids that support sperm. A volume below 1.5 mL may also suggest incomplete sample collection or anatomical blockages.
- Testing: Semen volume is measured by weighing the sample or using a graduated pipette. It provides a baseline for the rest of the analysis.
- Sperm Concentration
- What It Measures: Sperm concentration measures the number of sperm per milliliter of semen. Normal values typically exceed 15 million sperm per mL.
- Why It Matters: Low sperm concentration, or oligospermia, may indicate hormonal imbalances, testicular issues, or genetic factors. This information is vital for determining potential fertility treatments, such as assisted reproductive technologies (ART).
- Testing: Concentration is assessed manually by counting sperm under a microscope or using CASA, which provides automated and consistent measurements.
- Total Sperm Count
- What It Measures: Total sperm count is the number of sperm in the entire ejaculate, calculated by multiplying sperm concentration by semen volume.
- Why It Matters: Total sperm count helps assess whether there’s an adequate amount of sperm present to increase the likelihood of conception. A count below 39 million per ejaculate may suggest fertility challenges.
- Testing: Total count is derived from concentration and volume, offering a broader look at sperm production capacity.
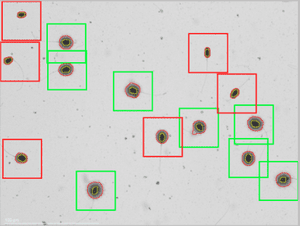
- Motility
- What It Measures: Sperm motility is the ability of sperm to move properly toward an egg. It’s divided into progressive motility (sperm moving forward effectively) and non-progressive motility (sperm that move but not effectively forward).
- Why It Matters: Poor motility, or asthenozoospermia, means sperm may struggle to reach and fertilize an egg, reducing the chances of conception. Assessing motility helps determine if fertility treatments like intrauterine insemination (IUI) or in vitro fertilization (IVF) with intracytoplasmic sperm injection (ICSI) are appropriate.
- Testing: Motility is evaluated manually using a microscope, often in conjunction with CASA, which can track and quantify movement patterns accurately. The World Health Organization (WHO) Laboratory Manual recommends assessing at least 200 sperm to achieve accurate motility results.
- Morphology
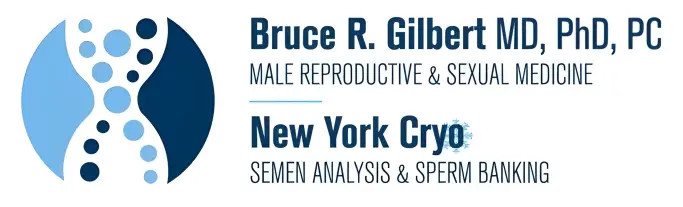
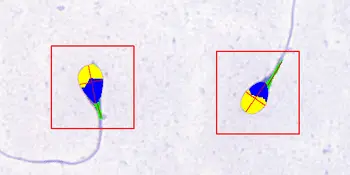
- What It Measures: Morphology examines the shape and structure of sperm, including the head, midpiece, and tail. Typically, at least 4% of sperm should have a normal shape.
- Why It Matters: Abnormal sperm shape, or teratozoospermia, may impair the sperm’s ability to penetrate the egg, reducing fertility. Morphology is crucial for determining treatment, especially for IVF, where morphology can predict fertilization success rates.
- Testing: Morphology is analyzed manually by trained technologists or via CASA. The Kruger or WHO strict criteria are used to evaluate normal and abnormal sperm shapes, with CASA providing more objective assessments.
- Vitality
- What It Measures: Vitality measures the percentage of live sperm in the sample, which helps differentiate between immotile (non-moving) and dead sperm.
- Why It Matters: Vitality is especially useful when motility is low. If many sperm are alive but immotile, there may be issues with the sperm’s flagella (tail) rather than viability, which can help guide treatment.
- Testing: Vitality is assessed by staining the sample to distinguish live from dead sperm.
- pH
- What It Measures: Semen pH indicates the acidity or alkalinity of the sample, which is typically between 7.2 and 8.0.
- Why It Matters: Low pH can signal blockages or infections in the reproductive tract, affecting sperm health and function.
- Testing: pH is measured with test strips or pH meters, with any abnormal findings prompting further investigation.
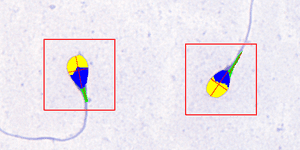
- Leukocyte (White Blood Cell) Count
- What It Measures: A high white blood cell count (leukocytospermia) may indicate infection or inflammation.
- Why It Matters: Inflammation can damage sperm DNA, impacting fertility. Identifying leukocytospermia allows for targeted treatments, such as antibiotics or anti-inflammatory medications.
- Testing: Leukocytes are identified manually with staining techniques or using CASA, which can highlight the presence of non-sperm cells in the sample.
Manual vs. CASA Analysis
- Manual Analysis: Performed by trained laboratory technologists using a microscope, the manual analysis provides detailed assessments, especially for morphology and motility. However, it requires extensive training and skill for accuracy. Many labs, especially commercial labs, have few trained andrology technologists. This can result in variable precision and accuracy in the reported results.
- CASA (Computer-Aided Sperm Analysis): CASA uses automated software to assess sperm count, motility, and morphology. CASA provides consistency and reduces variability between samples, which is beneficial for tracking treatment outcomes.
The Importance of a Specialized Andrology Laboratory
A specialized licensed andrology laboratory offers several advantages over general laboratories:
- Qualified Technologists: Laboratories specializing in semen analysis employ technologists trained specifically in sperm analysis, reducing errors and enhancing reliability.
- Strict Protocols: Licensed labs follow standardized protocols, such as the WHO Laboratory Manual for the Examination and Processing of Human Semen, ensuring that results are consistent and comparable.
- Image and Video Documentation: High-quality labs provide documentation of sperm images and videos, allowing results to be reviewed in case of questions or to confirm analysis accuracy.
Semen Analysis in Diagnosis and Treatment
Semen analysis plays a vital role in diagnosing male factor infertility:
- Combined with Blood Tests: Blood tests can reveal hormonal imbalances or underlying conditions affecting fertility, while semen analysis focuses on sperm health and quality.
- Alongside Imaging Studies: Imaging tests, such as scrotal ultrasound, can detect structural issues, like varicoceles or blockages, that affect sperm production. Together, these tests help pinpoint the cause of infertility.
- Guiding Treatment Options: Results from semen analysis help healthcare providers decide on the most suitable fertility treatments, such as IUI, IVF, or IVF with ICSI. For example, if motility is low but sperm count is high, ICSI may be preferred, as it bypasses the need for sperm to reach the egg naturally.
Semen analysis is a cornerstone of male fertility evaluation, offering crucial insights into sperm health and guiding targeted treatment options. By examining components such as sperm count, motility, morphology, and vitality, this analysis sheds light on potential causes of male factor subfertility and directs the next steps in care. A reliable and comprehensive analysis—performed in a licensed andrology laboratory by qualified technologists—ensures the highest accuracy and confidence in results. Together with blood testing and imaging studies, semen analysis forms an essential part of a holistic approach to diagnosing and treating fertility issues, helping patients and healthcare providers make informed decisions. As we move to Part 4: Imaging Studies, we’ll explore how imaging complements these evaluations, adding another dimension to our understanding of male fertility.
References
- World Health Organization. “WHO Laboratory Manual for the Examination and Processing of Human Semen,” 6th Edition.
- Esteves SC, et al. “Diagnostic evaluation of the infertile male: A committee opinion.”
- Cooper TG, et al. “Semen analysis standards and thresholds: re-evaluating the WHO criteria.”