PRESERVING FERTILITY IN KLINEFELTER’S PATIENTS
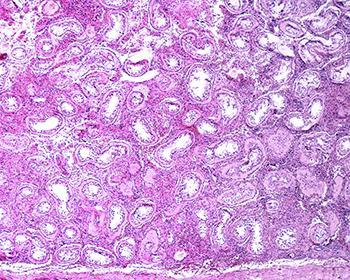
Klinefelter syndrome (KS) is one of the most common chromosomal abnormalities, affecting approximately 1 in 500 to 1 in 1,000 males. KS is typically characterized by an extra X chromosome, resulting in a karyotype of 47,XXY, though variants exist. One of the most significant clinical features of KS is infertility, with over 95% of KS patients being azoospermic (having no sperm in the ejaculate). This infertility arises because of progressive degeneration of the seminiferous tubules and Sertoli cells, which ultimately leads to a depletion of germ cells, the precursors to sperm. However, advances in reproductive medicine have offered new hope for fertility preservation in these individuals, particularly through early interventions.
In this blog, we will explore the fertility preservation strategies in pre-pubertal and post-pubertal KS patients, discussing the realistic expectations for sperm retrieval and recent controversies in the field. We will review the latest literature to provide a comprehensive understanding of what fertility preservation entails for KS patients at different life stages.
Pre-pubertal Fertility Preservation in Klinefelter’s Syndrome Patients

Pre-pubertal fertility preservation is a growing area of interest for KS patients, given that the loss of germ cells begins in childhood, well before puberty. The primary aim of pre-pubertal interventions is to preserve the spermatogonia (early-stage sperm cells) before the degenerative process accelerates during puberty. While techniques for preserving fertility in pre-pubertal boys are still experimental, there are promising avenues being explored.
Testicular Tissue Cryopreservation
One of the most investigated strategies for pre-pubertal KS patients is testicular tissue cryopreservation. This technique involves the removal and freezing of testicular tissue that contains spermatogonial stem cells (SSCs). These cells have the potential to mature into functional sperm once cultured or transplanted into the patient’s testes later in life. Though there are no established clinical protocols for SSC transplantation or in vitro maturation in humans yet, animal studies have shown promising results.
However, there are ethical and logistical challenges associated with testicular tissue cryopreservation in children. The primary concern is that the technique is still experimental, meaning that families and clinicians must weigh the potential benefits against the unknowns of future success rates. The question of when and how to use the preserved tissue remains unresolved.
Current Recommendations for Pre-pubertal Patients
At present, most fertility specialists suggest that testicular tissue cryopreservation be offered only as part of a clinical trial. Parents of KS boys who are interested in fertility preservation should be counseled on the experimental nature of this technique and the current lack of human data on successful outcomes. The procedure may offer hope, but the long-term viability of using preserved tissue for future fertility remains to be seen.
Post-pubertal Fertility Preservation in Klinefelter’s Syndrome Patients
Once KS patients reach adolescence and adulthood, fertility preservation becomes more challenging because of the progressive degeneration of germ cells and the accompanying fibrosis of the testicular tissue. Despite this, there are still options for sperm retrieval and cryopreservation in post-pubertal KS individuals.
Sperm Retrieval Techniques
- Testicular Sperm Extraction (TESE): Testicular sperm extraction (TESE) is the most widely used technique for attempting sperm retrieval in KS patients. During TESE, small portions of testicular tissue are surgically removed, and any sperm found within the tissue are extracted and cryopreserved. This technique is more effective when performed in adolescence or early adulthood, before the testicular tissue has undergone significant fibrosis.
- Microdissection TESE (micro-TESE): Micro-TESE is a more advanced technique where a high-powered microscope is used to identify areas of the testis that are most likely to contain sperm. Studies have shown that micro-TESE has higher success rates compared to conventional TESE, with sperm retrieval rates ranging from 30% to 60% in KS patients. However, success is still highly dependent on the patient’s age and the extent of testicular degeneration.
Hormonal Therapy to Improve Sperm Retrieval
There is emerging evidence that hormone therapy may enhance the chances of successful sperm retrieval in KS patients. The most common approach is administering selective estrogen receptor modulators (SERMS), aromatase inhibitors (AI), human chorionic gonadotropin (hCG) or follicle-stimulating hormone (FSH) to stimulate the testes and promote spermatogenesis. Some studies have suggested that hormonal therapy given before TESE may improve sperm retrieval rates, but this remains a topic of debate. Moreover, testosterone replacement therapy, often used to manage symptoms of hypogonadism in KS patients, paradoxically inhibits sperm production, adding complexity to treatment decisions.
Cryopreservation of Retrieved Sperm
Once sperm are retrieved via TESE or micro-TESE, they can be cryopreserved for future use in assisted reproductive techniques, such as intracytoplasmic sperm injection (ICSI). It is important to note that KS patients often produce very small quantities of sperm, making ICSI the preferred method of fertilization. ICSI involves the direct injection of a single sperm into an egg, bypassing the need for large numbers of sperm.
Realistic Expectations for Sperm Retrieval
Understanding realistic expectations for sperm retrieval is crucial for KS patients and their families. While advances in sperm retrieval techniques, such as micro-TESE, have improved success rates, not all KS patients will have retrievable sperm, particularly those who undergo the procedure later in life.
Adolescents and Young Adults
In adolescents and young adults with KS, sperm retrieval rates are generally higher, ranging from 30% to 60%, depending on the technique used and the extent of testicular fibrosis. However, even in cases where sperm is successfully retrieved, the quantity is often limited. Thus, while fertility preservation is possible, spontaneous conception without assisted reproduction is exceedingly rare.
Adult Men
For KS patients in their 30s and 40s, sperm retrieval becomes more difficult due to increased testicular fibrosis and depletion of germ cells. Studies have shown that sperm retrieval rates in this age group drop significantly, with some reports indicating success rates as low as 5-10%. Therefore, it is critical for adult men with KS to have realistic expectations about their chances of achieving biological fatherhood.
Controversies and Ethical Considerations in Fertility Preservation for KS Patients
Fertility preservation in KS patients is not without controversy. One of the central debates revolves around whether pre-pubertal interventions, such as testicular tissue cryopreservation, should be routinely offered given the experimental nature of these techniques. Some clinicians argue that offering such procedures raises false hope for families, while others believe that they are a necessary step toward advancing the field and improving future outcomes.
Another contentious issue is the role of hormonal therapy in optimizing sperm retrieval. While some studies suggest that pre-treatment with, SERMS, AI, hCG or FSH can improve success rates, others argue the benefits are not well established, and there is a risk of delaying necessary procedures. Similarly, the use of testosterone replacement therapy in KS patients must be carefully managed, as it can further impair spermatogenesis.
Lastly, the psychological impact of fertility preservation on KS patients and their families should not be underestimated. The emotional toll of undergoing invasive procedures, combined with the uncertainty of success, can lead to stress and anxiety. Healthcare providers must offer counseling and support throughout the fertility preservation journey.
Recent Advances and Future Directions
Research into fertility preservation in KS patients is ongoing, with several exciting developments on the horizon. One promising area of research is in vitro maturation (IVM) of spermatogonial stem cells, which could potentially allow sperm to be produced from testicular tissue in the laboratory. While still in the experimental phase, this approach could revolutionize fertility preservation for KS patients.
Another area of interest is gene editing technologies, such as CRISPR, which could theoretically correct the genetic abnormalities in KS patients and restore normal spermatogenesis. However, these techniques are far from clinical application and raise significant ethical concerns.
Conclusion
Fertility preservation in Klinefelter’s syndrome patients is a complex and evolving field. While pre-pubertal interventions, such as testicular tissue cryopreservation, offer hope for future fertility, they remain experimental, and the outcomes are uncertain. In post-pubertal patients, sperm retrieval through techniques like micro-TESE can offer a chance at biological fatherhood, though success rates decline with age. It is essential for patients and their families to have realistic expectations and to be fully informed of the risks and benefits of fertility preservation strategies.
As research continues to advance, the future of fertility preservation in KS patients looks promising, but there is still much to learn. Ethical considerations, including the experimental nature of some interventions and the emotional impact on patients, must remain at the forefront of clinical decision-making.